1.儿童及青少年血糖控制目标 控制血糖可以延缓儿童和青少年1型糖尿病并发症的发生和进展,降糖治疗中既要使患者血糖达标,又要注意治疗过程中尽量避免发生严重低血糖造成儿童认知功能障碍。有关控制目标和降糖策略的制定应根据个体化原则。具体目标血糖推荐值见表2-19。
表2-19 儿童和青少年1型糖尿病目标血糖推荐值

2.老年糖尿病患者血糖控制目标 老年人(根据我国标准为≥60岁)是糖尿病的主要患病人群。2007—2008年全国糖尿病调査报告数据显示,60岁以上老年人中糖尿病患病率为20.4%,估算约为3 538万,占总患病人数的38.1%。老年糖尿病血糖控制目标应遵循个体化的原则,选择不同的控制目标,目前倾向于根据患者年龄、伴发疾病情况,以患者HbA1c值作为衡量标准。
(1)HbA1c<7.5%:适用于预期生存期>10年、较轻并发症及伴发疾病,有一定低血糖风险,应用胰岛素促泌剂类降糖药物或以胰岛素治疗为主的2型和1型糖尿病患者。
(2)HbA1c<8.0%:适用于预期生存期>5年、中等程度并发症及伴发疾病,有低血糖风险,应用胰岛素促泌剂类降糖药物或以多次胰岛素注射治疗为主的老年糖尿病患者。
(3)HbA1c<8.5%:如有预期寿命<5年、完全丧失自我管理能力等情况,HbA1c的控制标准可放宽至<8.5%,治疗过程中尽量不出现严重高血糖(>16.7mmol/L),以避免糖尿病急性并发症和感染等情况发生。
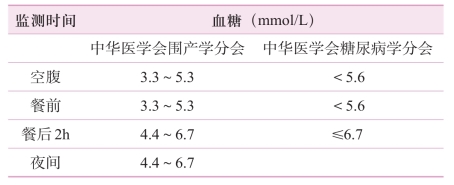
3.妊娠糖尿病患者血糖控制目标 2001年,美国国立卫生研究院在全球范围内进行了一项多中心的前瞻性研究,即“高血糖与不良妊娠结局研究(HAPO)”。HAPO结果表明,妊娠期轻度高血糖就可以造成母儿妊娠不良结局风险增加,严格的血糖管理可显著改善母儿结局。因此近年来对于妊娠期间血糖控制要求更为严格。具体控制目标见表2-20。
表2-20 妊娠期间血糖控制目标
4.住院患者血糖控制目标 近年来,住院患者中合并糖尿病比例明显升高,对于不同病情住院患者,应制定个体化的血糖控制目标。一般情况下,糖尿病患者住院期间血糖不一定要达标;降糖治疗应尽量避免低血糖,尽量避免超重及肥胖患者体重增加;另外,不能过度放松血糖管理而增加感染和高血糖危象的风险。具体血糖控制目标如下。
(1)非手术住院患者。
1)新诊断、病程较短、无并发症和严重伴发疾病的非老年(<65岁)糖尿病患者:若降糖治疗无低血糖及体重增加等不良反应,且有医疗条件和健康需求,依从性好,采用严格标准,即空腹或者餐前血糖控制在4.4~6.0mmol/L,餐后2h血糖或任意时点血糖为6~8mmol/L。
2)低血糖高危人群:糖尿病病程>15年、有低血糖病史、有严重伴发病如肝肾功能不全或全日血糖波动大并反复出现低血糖症状的患者,住院治疗期间加强血糖监测,避免低血糖的发生,血糖控制采用宽松标准,即空腹或者餐前血糖为8~10mmol/L,2hPG或任意时点血糖为8~12mmol/L,甚至最高血糖可放宽至13.9mmol/L。
3)心脑血管疾病患者及心脑血管疾病高危人群:对已患有心脑血管疾病的患者,采用宽松目标,即空腹或者餐前血糖8~10mmol/L,2hPG或任意时点血糖水平8~12mmol/L,可放宽至13.9mmol/L。对心脑血管疾病高危人群,采用一般标准,即空腹或餐前血糖6~8mmol/L,2hPG或任意时点不能进食血糖水平8~10mmol/L。
4)其他特殊人群:①肝肾功能不全患者,空腹或餐前血糖在8~10mmol/L,2hPG或任意时点不能进食血糖水平8~12mmol/L,最高血糖可放宽至13.9mmol/L。②糖皮质激素治疗患者:采用一般标准,即空腹或餐前血糖6~8mmol/L,2hPG或不能进食时任意时点血糖水平8~10mmol/L。③老年患者,年龄≥80岁的患者,采用宽松标准,即空腹或餐前血糖8~10mmol/L,2hPG或不能进食时任意时点血糖水平8~12mmol/L,最高血糖可放宽至13.9mmol/L。④预期寿命<5年患者,如癌症、精神或智力障碍、老年独居、胃肠外营养或胃肠营养等,采用宽松标准,即空腹或餐前血糖8~10mmol/L,2hPG或不能进食时任意时点血糖水平8~12mmol/L,最高血糖可放宽至13.9mmol/L。
(2)ICU患者血糖控制目标:ICU包括外科ICU(SICU)及内科ICU(M ICU),血糖控制目标采用宽松标准,即空腹或餐前血糖8~10mmol/L,2hPG或任意时点不能进食血糖水平8~12mmol/L。
5.围手术期患者血糖控制目标
(1)择期手术:要求术前HbA1c<8.5%。术前、术中及术后血糖控制目标,采用宽松标准,即空腹或餐前血糖8~10mmol/L,2hPG或任意时点不能进食血糖水平8~12mmol/L,短时间<15mmol/L也可接受。
对非老年患者,如身体状况良好,无心脑血管疾病并发症风险,或单纯应激性高血糖,可采用一般标准,即空腹或餐前血糖6~8mmol/L,2hPG或任意时点不能进食时血糖水平8~10mmol/L。
(2)精细手术(如整形手术等):采用严格标准,即空腹或餐前血糖4.4~6.0mmol/L,2hPG或不能进食时血糖水平6~8mmol/L。
(3)器官移植手术:采用一般标准,即空腹或餐前血糖6~8mmol/L,2hPG或任意时点血糖水平8~10mmol/L。
(4)急诊手术:术中及术后血糖控制目标与相应手术类型的择期手术术中及术后控制目标相同。
(林毅)
参·考·文·献
[1]KlemettiM M,LaivuoriH,Tikkanen M,etal.White's classification and pregnancy outcome in women w ith type 1 diabetes:a population-based cohort study[J].Diabetologia,2016,59(1):92-100.
[2]Grigorakis S I,AlecizakiM,BeisC,etal.Hormonal Parameters in Gestational Diabetesmellitusduring the third trimester:high glucagon levels[J].Gynecol Obstet Invest,2000,49:106-109.
[3]Imagawa A,Hanafusa T,Uchigata Y,et al.Fulm inant type 1 diabetes:a nationwide survey in Japan[J].DiabetesCare,2003,26:2345-2352.
[4]Shimizu I,Makino H,Imagawa A,etal.Clinical and immunogenetic characteristicsof fulminant type 1 diabetesassociated w ith pregnancy[J].JClin EndocrinolMetab,2006,91:471-476.
[5]Ben H A,Yogev Y,Hod M.Epidemiology of gestational diabetesmellitusand itsassociationwith type2 diabetes[J].DiabetMed,2004,21(2):103-113.
[6]Sivan E,Bod en G.Free fatty acids,insulin resistance,and pregnancy[J].Curr Diab Rep,2003,3(4):319-322.
[7]Wolf M,Sauk J,Shah A,eta1.Inflammation and glucose intolerance:a prospective study of gestational diabetesmellitus[J].Diabetes Care,2004,27(1):21-27.
[8]Megia A,Gallart L,Fernandez R JM,et al.Mannose-binding lectin gene polymorphisms are associated w ith gestational Diabetesmellitus[J].JClin EndocrinolMetab,2004,89(10):5081-5087.
[9]Qiu C,Sorensen TK,Luthy DA,etal.A prospective study ofmaternalserum C-reactive protein(CRP)concentrations and risk of gestational diabetes mellitus[J].Paediatr PerinatEpidemiol,2004,18(5):377-384.
[10]Tamas G,Kerenyi Z.Current controversies in themechanisms and treatment of gestational diabetes[J].Curr Diab Rep,2002,2(4):337-346.
[11]WilliamsM A,Oiu C,Muy RM,etal.Plasma adiponectin concentrations in early pregnancy and subsequent risk of gestational diabetesmellitus[J].J Clin EndocrinolMetab,2004,89(5):2306-2311.
[12]Winzer C,Wagner O,Festa A,et al.Plasma adiponectin,insulin sensitivity and subclinical inflammation in women w ith prior gestational diabetes mellitus[J].DiabetesCare,2004,27(7):1721-1727.
[13]Qiu C,M ichelle A,Vadachkoria S,etal.Increasedmaternal plasma leptin in early pregnancy and risk of gestational diabetes mellitus[J].Obstet Gynecol,2004,103(3):519-525.
[14]Lappas M,Permezel M,Rice G E.Release of proinflammatory cytokines and 8-isoprostane from placenta,adipose tissue,and skeletalmuscle from normal pregnantwomen and women with gestational diabetesmellitus[J].J clin EndocrinolMetab,2004,89(11):5627-5633.
[15]HAPOStudy CooperativeResearch Group.Hyperglycemiaand adverse pregnancy outcomes[J].New England Journal of Medicine,2008;358(19):1991-2002.
[16]American DiabetesAssociation.Diagnosisand classification of diabetesmellitus[J].DiabetesCare,2011.34(Suppl1):S62-S69.
[17]American DiabetesAssociation.Diagnosisand classification of diabetesmellitus[J].DiabetesCare,2014,37:S81-S90.
[18]中华医学会妇产科学分会产科学组,中华医学会围产医学分会妊娠合并糖尿病协作组.妊娠合并糖尿病诊治指南(2014)[J].中华妇产科杂志,2014.(49)8,561-568.
[19]InternationalAssociation Of DiabetesAnd Pregnancy Study Groups Consensus Panel.International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy[J].DiabetesCare,2010,33(3):676-682.
[20]Gupta Y,Kalra B,Baruah M P,et al.Updated guidelines on screening for gestationaldiabetes[J].Int JWomensHealth.2015,7:539-550.
[21]Cooper W O,Hernandez-Diaz S,Arbogast P G,et al.Major congenital malformations after first-trimester exposure to ACE inhibitors[J].N Engl J Med,2006,354:2443-2451.
[22]Quan A.Fetopathy associated w ith exposure to angiotensin converting enzyme inhibitors and angiotensin receptor antagonists[J].Early Hum Dev,2006,82:23-28.
[23]Velázquez-Armenta E Y.AngiotensinⅡreceptor blockers in pregnancy:a case reportand systematic review of the literature[J].Hypertens Pregnancy,2007,26:51-66.
[24]Bullo M,Tschum i S,Bucher B.Pregnancy outcome follow ing exposure to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists:a systematic review[J].Hypertension,2012,60:444-450.
[25]Edison R J,MuenkeM.Mechanistic and epidem iologic considerations in the evaluation of adverse birth outcomes follow ing gestational exposure to statins[J].Am JMed GenetA,2004,131:287-298.
[26]Kazm in A,Garcia-Bournissen F,Koren G.Risks of statin use during pregnancy:a systematic review[J].JObstetGynaecolCan,2007,29:906-908.
[27]Callaway L K,Prins JB,Chang A M,et al.The prevalence and impact of overweightand obesity in an Australian obstetric population[J].Med JAust,2006,184:56-59.
[28]Crane JM,White J,Murphy P,etal.The effectof gestationalweightgain by bodymass index onmaternal and neonatal outcomes[J].JObstetGynaecol Can,2009,31:28-35.
[29]Tennant PW,Rankin J,Bell R.Maternal body mass index and the risk of fetal and infant death:a cohort study from the North of England[J].Hum Reprod,2011,26:1501-1511.
[30]Bhattacharya S,CampbellDM,ListonW A,etal.Effectofbodymass index on pregnancy outcomes in nulliparous women delivering singleton babies[J].BMCPublic Health,2007,7:168.
[31]InstituteofMedicine Dietary Reference Intakes:Energy,Carbohydrate,Fiber,Fat,Fatty Acids,Cholesterol,Protein,and Amino Acids.Washington,DC:NationalAcademies Press;2002.
[32]IOM(Institute of Medicine)and NRC(NationalResearch Council).Weight Gain During Pregnancy:Reexam ining the Guidelines.Washington,DC:The NationalAcademies Press;2009.
[33]Price N,Bartlett C,Gillmer M.Use of insulin glargine during pregnancy:a case-controlpilotstudy[J].BJOG,2007,114:453-457.
[34]Fang YM,MacKeen D,Egan JF,etal.Insulin glargine compared w ith neutral protamine Hagedorn insulin in the treatmentof pregnant diabetics[J].J Matern FetalNeonatalMed,2009,22:249-253.
[35]Sm ith JG,Manuck T A,White J,Merrill D C.Insulin glargine versus neutral protamine Hagedorn insulin for treatment of diabetes in pregnancy[J].Am JPerinatol,2009,26:57-62.
[36]Egerman R S,Ramsey R D,Kao LW,etal.Perinatal outcomes in pregnanciesmanaged w ith antenatal insulin glargine[J].Am JPerinatol.2009,26:591-595.
[37]Langer O,Conway D L,BerkusM D,etal.A comparison of glyburide and insulin in womenw ith gestationaldiabetesmellitus[J].N Eng JMed,2000,343:1134-1138.
[38]Langer O,Yogev Y,Xenakis E M,et al.Insulin and glyburide therapy:dosage,severity level of gestational diabetes,and pregnancy outcome[J].Am JObstetGynecol,2005,192:134-139.
[39]Lord JM,Flight IH,Norman R J.Insulin-sensitizing drugs(metform in,troglitazone,rosiglitazone,pioglitazone,D-chiro-inositol)for polycystic ovary syndrome[J].Cochrane Database SystRev,2003,3(3):CD003053.
[40]Nanovskaya T N,Nekhayeva IA,Patrikeeva S L,et al.Transfer ofmetfor-min across the dually perfused human placental lobule[J].Am JObstetGynecol,2006,195:1081-1085.
[41]Rowan JA,Hague W M,Gao W,et al.Mefformin versns insulin for the treatmentofgestationaldiabetes[J].N Engl JMed,2008,358:2003-2015.
[42]Balani J,Hyer S L,Rodin D A,et al.Pregnancy outcomes in women w ith gestational diabetes treated w ith metformin or insulin:a case-control study[J].DiabetMed,2009,26:798-802.
[43]Silva JC,Pacheco C,Bizato J,etal.Metform in compared w ith glyburide for themanagementof gestational diabetes[J].Int JGynaecnl Obstet,2010,11(1):37-40.
[44]BertiniAM,Silva JC,TabordaW,etal.Pefinatal outcomes and the use of oralhypoglycem ic agents[J].JPefinatMed,2005,33:519-523.
[45]Graves CR.Antepartum fetalsurveillanceand tim ing of delivery in the pregnancy complicated by diabetesmellitus[J].Clin ObstetGynecol,2007,50:1007-1013.
[46]Hawkins S,Casey B M.Labor and delivery management for women w ith diabetes[J].Clin NAm ObstetGynecol,2007,34,323-334.
[47]Witkop C T,Neale D,Wilson L M,et al.Active compared with expectant delivery management in women w ith gestational diabetes:a systematic review[J].ObstetGyneeol,2009,113:206-217.
[48]Balsells M,Corcoy R,Adelantado JM,etal.Gestational diabetesmellitus:metabolic controlduring labour[J].DiabetesNutrMetab,2000,13:257-262.
[49]Gunderson E P.Breastfeeding after gestational diabetes pregnancy:subsequentobesity and type 2 diabetes inwomen and their offspring[J].Diabetes Care,2007,30:S161-S168.
[50]BeRamy L,Casas JP,Hingorani A D,el al.Type 2 diabetesmellitus after gestationaldiabetes:asystematic review andmeta-analysis[J].Lancet,2009,373:1773-1779.
[51]Kim C,New ton K M,Knopp RH.Gestational diabetesand the incidence of type 2 diabetes:a systematic review[J].Diabetes Care,2002,25:1862-1868.
[52]Rather R E,Christophi C A,Metzger B E,et al.Prevention of diabetes in women w ith a history of gestational diabetes:effects of metfomain and lifestyle interventions[J].JClin EndocrinolMetab,2008,93:4774-4779.
[53]Comm ittee on Obstetric Practice.ACOG comm ittee opinion No.435:postpartum screening for abnormal glucose tolerance in women who had gestational diabetesmellitus[J].ObstetGynecol,2009,113:1419-1421.
[54]吴红花,孙伟杰,惠岩,等.妊娠期糖代谢异常患者产后6~12周糖代谢转归的随访研究[J].中国糖尿病杂志,2009,1:466-469.
[55]AgarwalM M,Hughes PF,Punnose J,etal.Gestational diabetes screening of amultiethnic,high-risk population using glycated proteins[J].Diabetes ResClin Pract,2001,51(1):67-73.
[56]Xu Y,Wang L,He J,et a1.Prevalence and control of diabetes in Chinese adults[J].JAMA,2013,310:948-959.
[57]中华医学会糖尿病学分会慢性并发症调查组.1991~2000年全国住院糖尿病患者慢性并发症及相关大血管病变回顾性分析[J].中国医学科学院学报,2002,24:447-451.
[58]李晨曦,田慧,李春霖,等.综合管理对老年2型糖尿病患者血糖控制达标的促进作用[J].中华保健医学杂志,2011,13(2):113-116.
[59]王伟文.影响糖尿病患者药物治疗依从性相关因素临床分析[J].上海医药,2009,30(3):133-134.
[60]俞银燕,田慧,方福生,等.门诊2型糖尿病合并代谢综合征患者的综合控制达标情况及影响因素调查[J].中华保健医学杂志,2010,12(6):427-430.
[61]卢维晟,潘志红.老年2型糖尿病发病机制与诊治的新进展[J].上海医药,2012,(33):3-7.
[62]王全胜,李骏,刘晓丽,等.2型糖尿病并发低血糖昏迷患者的血糖控制应个体化[J].临床荟萃,2012,27(9):758-760.
[63]Asvold B O,Sand T,Hestad K,etal.Cognitive function in type 1 diabetic adults with early exposure to severe hypoglycemia:a 16-year follow-up study[J].DiabetesCare,2010,33(9):1945-1947.
[64]Whitmer RA,Karter A J,Yaffe K,etal.Hypoglycemic episodes and risk of dementia in older patientsw ith type 2 diabetemellitus[J].JAMA,2009,301(15):1565-1572.
[65]FeilDG,CatherineM L,David S.Quality Indicators for the Careof Dementia in Vulnerable Elders[J].JAm Geriatr Soc,2007,55(Suppl 2):S293-S301.
[66]中华医学会糖尿病学分会.中国2型糖尿病防治指南(2013)[J].中华内分泌代杂志,2014,30(10):893-942.
[67]中国老年学学会老年医学会老年内分泌代谢委员会.老年糖尿病诊疗措施专家共识(2013)[J].中华内科学杂志,2014,53(3):243-251.
[68]Kimbro L B,Mangione C M,Steers W N,et al.Depression and all-cause mortality in persons w ith diabetesmellitus:are older adults at higher risk?Results from the Translating Research Into Action for Diabetes Study[J].J Am Geriatr Soc,2014,62:1017-1022.
[69]James PA,Oparil S,Carter B L,etal.2014 evidence-based guideline for the management of high blood pressure in adults:report from the panel members appointed to the Eighth Joint National Comm ittee(JNC 8)[J].JAMA,2014,311:507-520.
[70]American DiabetesAssociation.OlderAdults-2015[J].DiabetesCare,2015,38(Suppl1):S67-S69.
[71]Kirkman M S,Briscoe V J,Clark N,etal.Diabetes in olderadults[J].DiabetesCare,2012,35:2650-2664.
[72]Tuomilehto J,Lindström J,Eriksson JG,etal.Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects w ith impaired Glucose tolerance[J].N Engl JMed,2001,344:1343-1350.
[73]Kimbro L B,Mangione C M,SteersW N,et al.Depression and all-cause mortality in persons w ith diabetesmellitus:are older adults at higher risk?Results from the translating research into action for diabetes study[J].JAm Geriatr Soc,2014,62:1017-1022.
[74]LiG,Zhang P,Wang J,etal.The long-term effectof lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study:a 20-year follow-up study[J].Lancet2008,371:1783-1789.
[75]Lindström J,Ilanne-Parikka P,Peltonen M,etal.Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention:follow-up of the Finnish Diabetes Prevention Study[J].Lancet,2006,368:1673-1679.
[76]Know lerW C,Fow ler SE,Hamman R F,etal.10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study[J].Lancet,2009,374:1677-1686.
[77]American DiabetesAssociation.Prevention or delay of type 2 diabetes-2015[J].DiabetesCare,2015,38(Suppl):S31-S32.
[78]Shah M,Kaselitz E,Heisler M.The role of community health workers in diabetes:updateon current literature[J].CurrDiab Rep,2013,13:163-171.
[79]中华人民共和国国家卫生和计划生育委员会.成人糖尿病患者膳食指导[M].北京:中国标准出版社,2013.
[80]万东君,罗晓红,王春雨.诱导2型糖尿病的蜜月期——治疗糖尿病的新策略[J].医学与哲学:临床决策论坛版,2009,30(9):55-56.
[81]Holman R R,Paul S K,Bethel M A,et al.10-year follow-up of intensive glucose control in type 2 diabetes[J].N Engl JMed,2008,359:1577-1589.
[82]田慧,李春霖,杨光.二甲双胍在老年2型糖尿病患者应用的安全性评估[J].中华内科杂志,2008,47(11):914-918.
[83]中华医学会糖尿病学分会.中国2型糖尿病防治指南(2013年版)[J].中国糖尿病杂志,2014,22(8):2-42.
[84]Duncan A E.Hyperglycem ia and perioperative glucosemanagement[J].Curr Pharm Des,2012,18(38):6195-6203.
[85]Frisch A,Chandra P,Smiley D,etal.Prevalenceand clinicaloutcome of hyperglycemia in the perioperative period in noncardiac surgery[J].Diabetes Care,2010,33:1783-1788.
[86]Dhatariya K,Levy N,KilvertA,etal.NHSDiabetesguideline for theperioperativemanagement of the adult patient with diabetes[J].Diabetic Medicine,2012,29:420-433.
[87]王彤,肖新华.糖尿病患者围手术期的血糖管理[J].中华内分泌代谢杂志,2010,26(6):527-528.
[88]吕庆国,童南伟.《中国成人住院患者高血糖管理目标》专家共识解读[J].中国实用内科杂志,2013,33(12):939-942.
[89]Wong J,Zoungas S,W right C.Evidence-based Guidelines for perioperative managementof diabetes in cardiac and vascular surgery[J].World JSurg,2010,34:500-513.
[90]Mary E.Boyle Karen M.Insulin pump therapy in the perioperative period:a review of care after implementation of institutionalguidelines[J].Journalof Diabetes Scienceand Technology,2012,6(5),1016-1021.
[91]董心童,陶明哲.糖尿病患者围手术期血糖管理的研究进展[J].广州医药,2012,43(6):49-52.
免责声明:以上内容源自网络,版权归原作者所有,如有侵犯您的原创版权请告知,我们将尽快删除相关内容。